How Buspirone Mixed with Melatonin to Make an Antidepressant
, Volume , Number ,
https://www.thecarlatreport.com/#
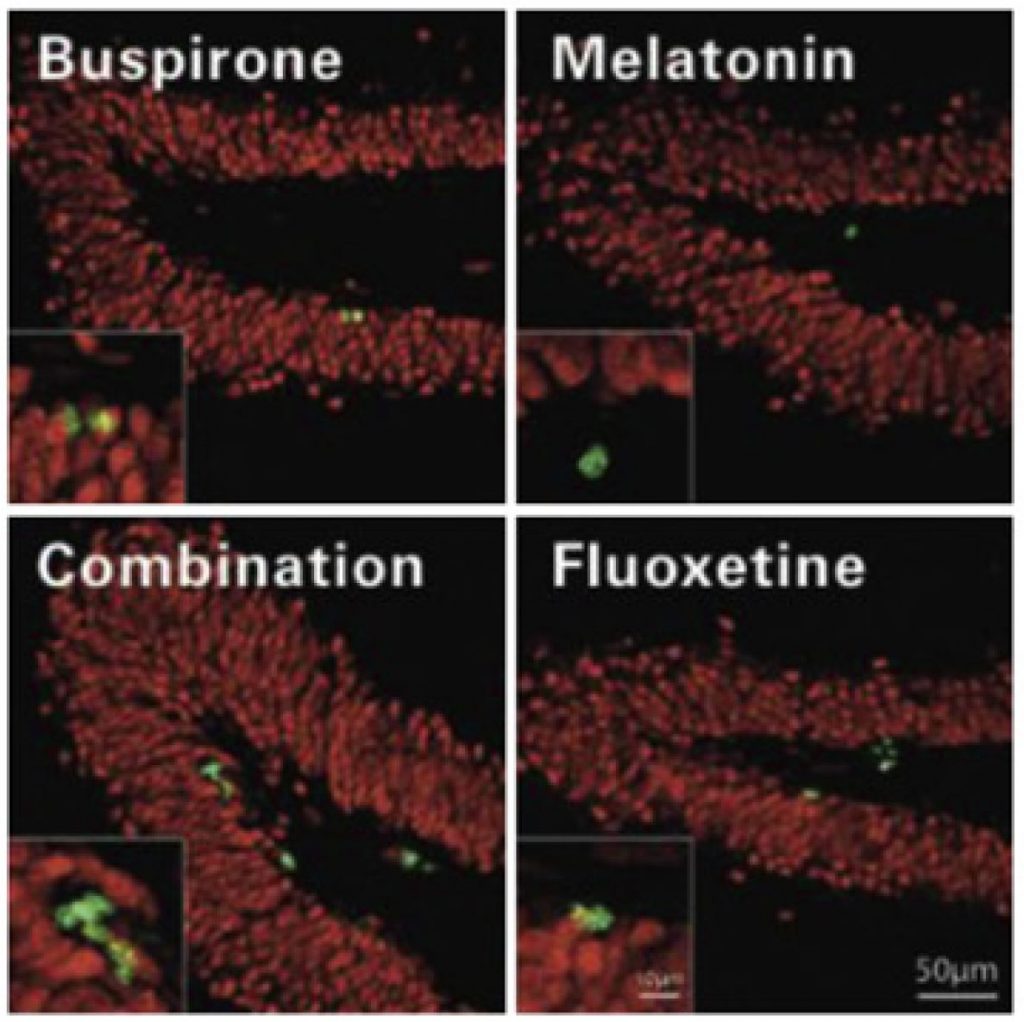
Published On: 2/21/2021 Duration: 19 minutes, 49 seconds Transcript: Buspirone (Buspar) is FDA approved for generalized anxiety disorder, and it hasn’t earned approval in any other conditions since its release by Bristol Meyers Squib in 1986. But we turned up some under-the-radar uses of buspirone in our February issue, and today we are going to focus on one of them: Depression. But first, some history. History of Buspirone Buspirone is generally classified as a serotonin 5-HT1A agonist, but when it was first synthesized in 1968 it was thought to have dopaminergic effects in high doses and they tried to develop it as an antipsychotic. That attempt failed, but researchers at Bristol Meyers Squibb kept testing the drug in animals. They saw what looked like antianxiety effects – mice who took buspirone were less aggressive and less fearful in the face of electric shocks. In 1979 the first human study of buspirone in anxiety was released – a randomized controlled trial that compared it to diazepam (Valium) and placebo. Both meds were dosed at around 20-25mg per day, divided 2-3 times a day. The authors – Drs. Goldberg and Finnerty, who also helped usher in trazodone – concluded that buspirone “was as effective an antianxiety agent as diazepam and produced no more and perhaps fewer side effects.” Other studies followed, but when it came time to submit them to the FDA there was a problem. All of the early studies were done with the DSM-II criteria for anxiety neurosis, but the field had moved on to DSM-III, where the closest thing was generalized anxiety disorder (GAD). So the researchers carried out some statistical back-peddling to pull GAD symptoms from the rating scales they used, and show that the drug probably worked in GAD as well. The FDA gave them a pass, and so buspirone was born in 1986. Studies in real GAD did follow after its release, but let’s take a look at the early criteria that buspirone was first discovered to work for: Anxiety neurosis “Anxiety neurosis is characterized by anxious over-concern extending to panic and frequently associated with somatic symptoms. Unlike Phobic neurosis, anxiety may occur under any circumstances and is not restricted to specific situations or objects. This disorder must be distinguished from normal apprehension or fear, which occurs in realistically dangerous situations.” And that’s the whole criteria. DSM III added a duration criterion – the anxiety had to last at least a month – and DSM IV extended that to 6 months. Generalized anxiety disorder also changed a lot from DSM-III to DSM-IV; the 1980’s style DSM-III listed a lot more physical symptoms than DSM-IV, and focused more on fear, apprehension, and hypervigiliance than everyday worries. How Busprione (Buspar) Works Buspirone treats anxiety without any benzo-like gabba effects. It is a serotonin 5-HT1A agonist, which is the same mechanism that fuels the anxiolytic properties of Silexan – the German extract of lavender that we reviewed for GAD last August. The antidepressants vilazodone (Vibryd) and vortioxetine (Trintellix) also share this mechanism, as do many atypical antipsychotics which are partial agonists at 5-HT1A, such as aripiprazole, asenapine, clozapine, lurasidone, quetiapine, and ziprasidone. Buspirone + Melatonin = An Antidepressant Buspirone is a popular augmentation strategy for antidepressants, but the research supporting that use is not as strong as its popularity would suggest. We get into that more in the online edition and identify a few reasons to use buspirone in depression. One of them is when buspirone is combined with melatonin. This is an interesting story of drug development. Two medications that don’t treat depression on their own – buspirone and melatonin – just might treat it when combined together. It all started ten years ago when Maurizio Fava’s group at Massachusetts General Hospital were screening drugs for their potential in depression. They did this by testing them in cell cultures of primitive, undifferentiated human brain cells to see if they caused cell growth, or neurogenesis. One cause of depression is shrinkage of brain cells in the hippocampus – most antidepressants increase cellular growth there, as does ECT and aerobic exercise, and blocking this neurogenesis renders antidepressants ineffective. Buspirone induced neurogenesis in this platform, but there was a problem. When they added it to the dish of undifferentiated brain cells, it caused those cells to develop into brain cells, but it also triggered them to develop into non-neuronal cells like astrocytes. This is not what they wanted; they wanted the neural growth effects to be concentrated in brain cells, especially in the hippocampus. So they looked for something they could add to buspirone to inhibit those other effects. One of their collaborators – Andrew Nierenberg – had published a case report in 2009 where he was able to treat treatment resistant bipolar depression with a combination of melatonin and low-dose buspirone, along with 75mg of bupropion. This lead to some thinking that buspirone and melatonin might have a unique antidepressant effect, so they ran the combination through the cell line, and it worked: The new combination caused neuronal growth, but not other kinds of cell growth. Next they tested it out in animals to get the dose just right. Why did they use low dose buspirone? They were aiming for as low a dose as possible to improve tolerability. Earlier studies had suggested that buspirone might have antidepressant effects at high doses, above 40mg/day, but most patients weren’t able to tolerate that, so in a way they were hoping to get those antidepressant effects at a lower dose through this melatonin synergy. The Human Study So they went from the petri dish – in vitro – to animals – in vivo – but what about in humans? The human study came next – 134 patients with moderate Major Depression volunteered to test the new combo therapy in a 6-week randomized controlled trial. Everyone either got placebo, buspirone 15mg, or the buspirone-melatonin combination – which was 15mg of buspirone and 3mg of melatonin SR. The melatonin the used was from Mellen Medical Products; it’s still available and affordable on their website. The buspirone-melatonin combo had a significant effect on the primary outcome – the clinical global improvement scale – as well as on secondary outcomes like overall CGI severity, Hamilton anxiety, and remission rates on the QIDS depression inventory, but not on the total QIDS score itself. So the combo did better than placebo, but did it do better than buspirone alone? Yes, it did better than both on all those measures. Buspirone did not work on any of them alone, not even anxiety, which is not too surprising since the dose was only 15mg/day. OK but I have a theory. What if this just proves that helping sleep with melatonin and helping anxiety with a little buspirone treats depression? I mean there are studies where eszopiclone (Lunesta) is added to an SSRI and it makes the SSRI work better – I’ve seen that in controlled trials of depression as well as generalized anxiety disorder. That’s a good theory, but in this case the melatonin didn’t actually improve any sleep items on the rating scale, so the thinking is that its antidepressant effects were due to some kind of pharmacodynamic synergy with buspirone – perhaps neurogenesis – rather than direct effects on sleep. On the other hand, they did look at cognitive symptoms in a separate study, and from that analysis it looks like improvements in cognition – rather than sleep – were driving the change in depression. When they compared patients who responded to the combo vs. those who did not, it was the change in cognitive symptoms that seemed to make the difference. That makes sense if we’re talking about a treatment that enhances growth in the hippocampus – the memory center. What specific cognitive symptoms did it help? Word-finding difficulties, forgetfulness, mental slowness, apathy and motivation. OK if I’m going to find a criticism of this study then it’s that it’s just one study – why hasn’t anyone tried to replicate it? That’s a mystery. I wrote to Dr. Fava who shared that his best guess is that there is no financial incentive here. If a company went through the trouble to license a combination pill with buspirone and melatonin in it, most physicians would bypass the combo pill by prescribing the two generic ingredients on their own. Their work on neurogenesis and depression has continued to yield fruit, however. After screening some 10,000 compounds through that neurogenesis cell line, they arrived at one with promise: NSI-189. It’s currently being developed for major depression by Neuralstem. The results have been mixed, but here’s something interesting – it seems to have better effects on cognition than on depression. OK so what’s the bottom line, should we use melatonin with buspirone? We tend to reserve these half-tested therapies for treatment resistant cases – and I would put it there at the end of the line along with other novel therapies like celecoxib, amantadine, minocycline, and D-cycloserine. But the buspirone-melatonin combo has two advantages: it is safe, and it improved cognition, which I wish we could say for more of our therapies. Buspirone’s Metabolite: 1-pyrimidinylpiperazine And now for the word of the day….1-pyrimidinylpiperazine Melatonin is not the only companion to help buspirone along. 1-pyrimidinylpiperazine – or 1PP for short – is an active metabolite of buspirone that is thought to contribute to its antianxiety effects. IPP is an antagonist of the α2-adrenergic receptor. Mirtazapien is also an α2 antagonist, as is yohimbine which – like buspirone – is frequently used to treat sexual dysfunction. 1PP made legal history when buspirone was slotted to go generic in 2000. Bristol Meyers Squibb, not wanting to let go of their blockbuster anxiety drug, attempted to hold onto it by patenting the metabolite 1PP. Copyrighting a metabolite is not unheard of – desvenlafaxine (Pristiq) is the active metabolite of venlafaxine (Effexor), but 1PP had been around a long time and was a metabolite of other drugs. Bristol Meyers Squibb, however, believed that they had proved that 1PP was necessary for buspirone’s therapeutic effects (in animal studies and in this human one), and that – by copyrighting this knowledge – they would prevent generic manufacturers from producing buspirone, because they would hold the copyright on the 1PP-buspirone combination that was created every time a patient swallowed the pill. The FDA would have none of this, however, and Buspar became generic buspirone in 2000. Attempts to extend the patent with a controlled release form were also explored, but these never came to market, although currently the generic manufacturer Mapi is trying to develop a controlled release buspirone, which would be a welcome advance for patients who have to take it 3 times a day. One thing to know about buspirone is that fluvoxamine blocks its metabolism, or conversion, into 1PP – the results is higher levels of buspirone – they are about doubled but fluvoxamine – and lower levels of 1PP – they are cut in half by fluvoxamine. So even if you adjust for this interaction but cutting the buspirone dose in half, you’ll still end up with a different mix of buspirone and its little helper: 1PP. A similar thing happens when bupropion (Wellbutrin) is added to most SSRIs except citalopram and escitalopram – and it’s these two –pram SSRIs that have the best evidence to work when augmented by bupropion. Article Referenced: “Buspirone: Still Effective After All These Years?“ The Carlat Psychiatry Report, February 2021 Got feedback? Take the podcast survey.
In 2012, psychiatrists at Harvard’s Massachusetts General Hospital discovered a novel antidepressant. It seemed to improve depression and cognition without causing any significant side effects. There was only one problem. The ingredients were practically free, and there was no way that was going to sell.





Leave A Comment
You must be logged in to post a comment.